Join Us to Help Celebrate National Pathology Week 2020!
Remember, Remember!
Remember, remember the fifth of November.
Gunpowder, treason and plot.
We see no reason
Why gunpowder treason
Should ever be forgot……
What can you do to help our scientists who’ve been sucked back in time to 1605 to find the gunpowder plotters and help Princess Elizabeth?
Full play on YouTube, scripts and activity packs are available here
Join in our digital competition, watch the play and complete the activity packs to help the Healthcare Science Education Team celebrate the work of Healthcare Scientists and the work they do for patients and families!
Watch the great play by Nicola Baldwin (2018) Remember, Remember! on our YouTube Channel (available Friday 30th October)
See how your hard work can help our scientists by completing the activity packs that accompany the show (download links below)
Also
Take photos, record a video or create other content (blog, tik tok, artwork etc) linked to your completed activities OR answers one of the following questions for a chance to win a £50 Amazon voucher!
– What do I think of when I hear the words microbiology / bug?
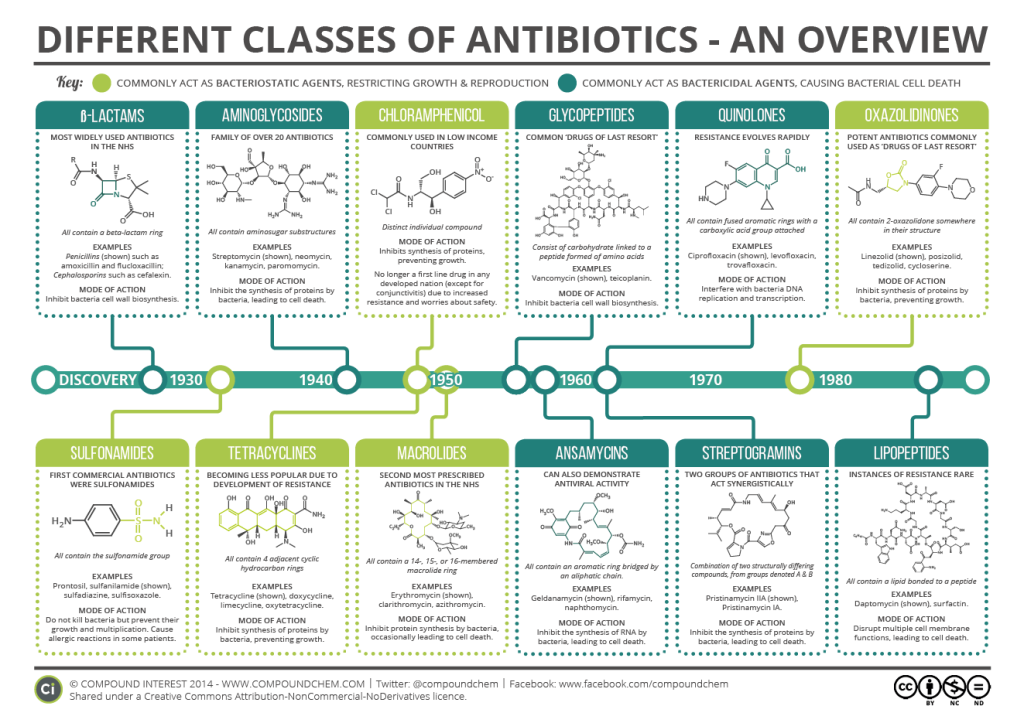
– What does antimicrobial resistance mean to me?
– What will antimicrobial resistance mean for my family?
– Are bugs good or bad?
– What do I think scientists do in hospitals?
Email: we transfer your entries to hcs.education@gosh.nhs.uk by Sunday 8th November
Lily, Rosa and Frank are Healthcare Scientists working in the laboratories. They work to help patients understand what is making them unwell, or to help with making them better.
It’s November and there is fog hanging in the air. The leaves have begun to fall and the street lights have started to come on by the time they leave work.
Scientists often work late into the night and Lily is waiting for Rosa and Frank to finish for the day.
Whilst waiting for them she decides to run one more test using her favourite piece of lab equipment, a MALDI-ToF she’s called Bonnie. Bonnie is a pretty cool piece of equipment: it has a laser and can get a result for Lily in less than 5 minutes for something she used to have to wait 2 days for.
Just as she presses the big red button, Rosa and Frank walk through the door to the laboratory. Suddenly a message appears on the screen, where no message should be saying ‘HELPE…’
Then the message changes and gives an address at the top of Lamb’s Conduit Street and what looks like a map.
Lily is so surprised she jumps back and tries to turn Bonnie off, but the machine doesn’t respond and the message just stays on the screen.
Not knowing what to do Lily, Rosa and Frank decide to leave the lab and find somewhere to sit and chat to work out what might have happened;, After all this is a piece of scientific equipment not a computer game.
As they leave the lab, they are suddenly surrounded by the fog they had seen outside the window until they can barely see what’s in front of them.
As they walk towards where they believe the tube to be, they suddenly realise they are on Lamb’s Conduit Street and the fog begins to clear.
A child is waiting. She has a Scottish accent and demands they call her Princess Elizabeth! They must all bow to her!
She tells them there is a plot to get rid of her father by blowing up the Houses of Parliament. The scientists are amazed – do you mean the Gunpowder Plot of 1605?
She says she will tell them later how she managed that.
Even then, they don’t believe she is a princess….
But she is
Remember, Remember! by Nicola Baldwin 2018
The scientists must find a way to help Princess Elizabeth find the Gunpowder Plotters. Then maybe they’ll be able to find out how to get back to 2020!
The scientists have asked you to complete a number of activities in order to help them find the plotters. You are the detectives, guiding the scientists so that they can get home.
Complete the following activities and we’ll find a way to get the results back in time to the scientists in 1605.