I’ve posted in previous years about what antimicrobials are, what antimicrobial resistance may mean for individuals, as well as some thoughts about how we might communicate around some of the challenges linked to antimicrobial resistance in a difference way, or plan our outreach differently. This year I wanted to sign post to some resources that I have either been involved with or found useful in order to help support both our own learning and planning responses to some of the common misconceptions about AMR I hear when I’m out and about talking to people.
What is antimicrobial resistance?
The World Health Organisation (WHO) talks about it like this:
Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi and parasites no longer respond to antimicrobial medicines. As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become difficult or impossible to treat, increasing the risk of disease spread, severe illness, disability and death.
I think it’s easy to forget that although AMR is a big part of the professional life of most Infection Control and microbiology professionals, even for other healthcare professionals it features less often, let alone for members of the public. It can be surprising therefore when you do go out and about, or even just talk to friends and family, to hear some of the ways that non infection professionals think about how AMR works and who it impacts.
Common misconceptions I hear when talking to people about AMR:
- It’s the body that becomes resistant to antibiotics
- I have never taken antibiotics so I cannot get a resistant infection
- Antibiotics treat all types of infection
- Antibiotics can be stopped when the symptoms stop
- Only infected patients can transmit antimicrobial resistance
If you reflect on some of these myths, it’s actually pretty easy to understand how they come about. Most people are focused on themselves and act from a human centric point of view. Many people give little, if any, thought to the multitudes of living bacteria that co-exist in their bodies. Once you accept this as the starting point, most of these myths are actually based on pretty small mental leaps. If, however, you don’t switch your point of view before you start having conversations about AMR, you can unwittingly end up reinforcing the very misconceptions you were aiming to address.
One of the reasons that I think this post is timely right now, is that I am already seeing more posts linked to how we should not be putting artificial medications into our bodies, alongside the back lash against vaccines, and so it seems to me a good time to remember what a difference these, now common, medical interventions have made to the lives of individuals and public health in general.

Let’s start with a little bit of context
Hardly any of us will have living memory of life without access to antibiotics and what life was like in a world without vaccination. One way to really get a feel for the impact these common interventions have made is to look at the impact in the last 30 years on reducing child mortality (death). Even in this recent time period, massive progress has been made due to advances such as the rota virus vaccine, but also in getting more global access to antimicrobial therapy where it is most needed.

Public health is multi factorial, with impacts being cumulative and made by more than just one thing, so not all of these impacts are made by antibiotic and vaccine availability. Other steps to reduce death linked to infectious disease include everything from clean water and sewer systems to pasteurisation and other means of food safety controls. The impact of these combined approaches is massive, but as the UN sustainable development goals show us, those of us who are access to clean water are not actually in the majority and more is yet to be done to ensure equality of access.

To aim to undo some if not all of this century plus of progress is something I find pretty hard to process. If you’ll forgive the momentary indulgence, I have to state that I think the current anti-vaccine and general anti medical stance that is being seen within some groups and communities is ultimately an act of extreme privilege It’s a privilege to be able to choose not to access something that is readily available to you and not available to others. It is a privilege not to have to live first hand the consequences of what the alternative might hold. It’s also a privilege to be able to change your mind and choose to access something later. Thinking of things in this light doesn’t necessarily help with having conversations in a supportive and open way when some of the underlying thinking may be so different, but it may mean we can flip the dialogue from one of imposition to one about the power of choice, and supporting evidenced based decision making for all.
Where does AMR come into this?
There’s a big stat that everyone quotes about more people dying from AMR than cancer by 2050, with an estimated 10 million deaths. As a scientist, I get the need to quantify and use numbers, as a human being however, I find that numbers that are so big can just be off-putting. They are so large it can make us, as individuals, feel powerless to impact them.
For me, the reason this conversation is so important to have in the right way, and pitched to the right communities, is because if we are going through a period of global push back against the common interventions, such as vaccination, that have successfully reduced mortality and provided first line protection, then our final line of defence in terms of treatment is now even more vital. 2050 isn’t that far away, and we are already seeing consequences linked to more resistant organisms being identified in severe infections. Therefore, the time to be having conversations and really raising awareness to impact decision-making is now. Sadly, this is coinciding with a period of time when trust in healthcare professionals and science in general feels very low. Instead of being defeated by this, however, we need to use it a driver to really focus on how we can do it better.
One of the other reasons that AMR is both important and challenging to communicate is that it is always in constant flux. You can’t just learn about it and move on. The mechanisms change, the diagnostics change, and the interplay of all of these factors within the bacterial host interactions can make it even more complex and hard to engage with. To exemplify this, the figure below was something I saw posted on Bluesky and fell in love with, as I adore the fact that it lists all kinds of routes to AMR in a single image, thus capturing the complexity of what we’re dealing with.

That said, you don’t have to understand all or any of this image to understand the core of why AMR is going to be a problem moving forward. The main thing to take away from it is that AMR is complicated, and as a result you will hear many different messages linked to it, and those messages will continue to change as we learn more and the impacts are felt differently. As a result, it can then sound like we don’t know what we’re doing, or just end up really off putting, as there isn’t one clear message we are getting out there for people to cling onto. We, therefore, need to build this flexibility into messages and link around core themes rather than trying to talk in absolutes. Otherwise, we risk losing more of the public confidence than has already occurred.
What is being done nationally?
This year, a new version of the UKs National Action Plan for confronting AMR has been released and within it there is a strong focus on the acknowledged need to educate both members of the public and healthcare professionals on AMR.
There is also plenty in there about increasing equitable access to antimicrobials, the need to improve diagnostics to help support both diagnostic and antimicrobial stewardship, and something that pleased me greatly, a special mention of the role of the built environment in managing AMR.
The thing is, top-down approaches will only ever get us so far. At some point, those of us involved in all things infection also need to be consciously including some of these drivers in our own every day practice.
No one can do everything, but whether you are collaborating with industry, undertaking research, or working in clinical practice, we have to embed AMR based action into our encounters. Do you include an AMR slide into all of your teaching? No matter the audience? Do you take the moment when it comes up with friends and family to just talk about the fact that this issue exists? Can you free up some capacity and undertake some public engagement?
Recognising there is a need is not the same thing as addressing that need, and we also have to be there to hold strategic partners and organisations to account in order to make sure action happens. So, let’s consciously match that top-down approach with a bottom-up drive for change.
What resources are there to help talk about AMR to other professionals
Having talked a lot about the need to talk to other healthcare professionals and seeing so much about #WAAW this year, it does really feel progress is being made to support us all to do this better.
Those of you who are UK based have probably heard of and support the Antibiotic Guardian programme (https://antibioticguardian.com/). This programme has lots of resources and supports personal action by asking you make a specific pledge about what you will undertake linked to addressing AMR.

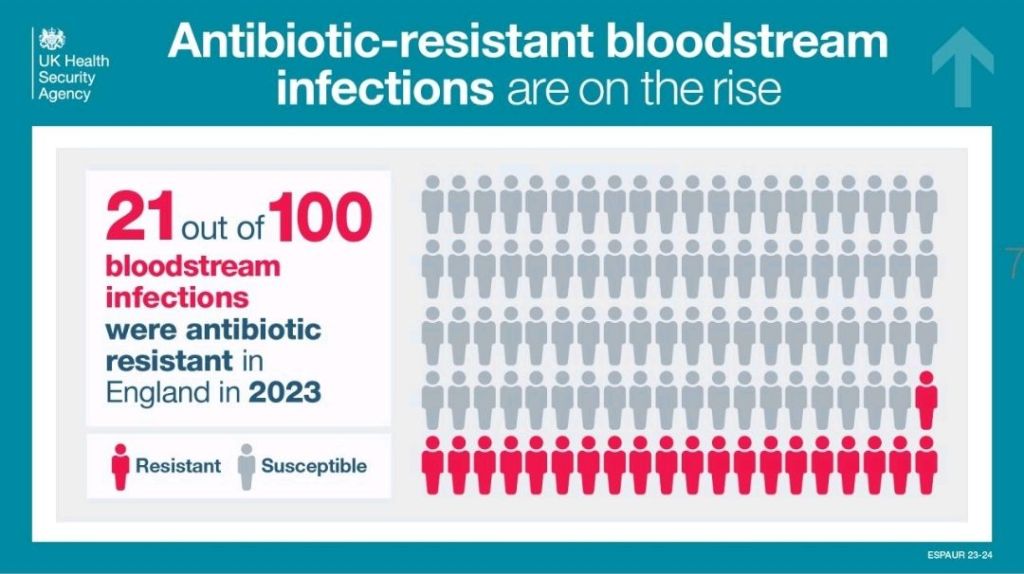
Every year, new infographics come out that talk about different aspects of AMR. Some of these, like the one above, link AMR into commonly known components of healthcare practice, such as hand hygiene, in order to support individuals to feel empowered to act. Others focus more on messaging about antibiotic courses, or as we heard a lot about at the FIS/HIS conference last week, things like IV to oral switches, and sending the right samples to enable a switch from broad to narrow spectrum antibiotics. There’s plenty of ones out there now that can be really useful to embed in talks or laminate and put up on walls. The UKHSA especially have recently released a lot for WAAW, and because there are so many, you can keep them on rotation so that they don’t just become invisible as people see them too frequently.
I’ve also been involved in creating various content this year, as have many others, including webinars and podcasts to explore some of the issues linked to AMR and provide different routes via which healthcare professionals can engage with information and CPD on this topic. I’ve included a link to just one of these below in case it’s of interest, but a quick internet search will provide you with all kinds of others.
https://www.selectscience.net/webinar/resistance-on-the-rise
The main thing to remember is that we all like to receive our learning in different ways, and so ensuring that we remember that when we’re designing our education strategies is one of the best ways to be impactful.
What resources are there to help talk about AMR to members of the public
The resources you might want to use linked to AMR will vary greatly based on your target audience. It’s important to remember that even if someone is a healthcare worker they are also a member of the public, and depending on their personal background or setting they work in, utilising content created for the general public may serve both purposes.
There is some really great video, podcast, infographic, blog, and other content aimed at public outreach on AMR. There’s even a musical called The Mold that Changed the World, about Fleming and Penicillin, as the first antibiotic.
There are lots of different entry points when you are thinking about content that might be appropriate, and you’re likely to go to different depths depending on whether you are doing a one off encounter or a more prolonged piece of relationship building.
The post that is linked to at the start of this article on AMR as a Super Wicked Problem may help with choosing your content. You may also want to consciously address some of the myths mentioned at the start or even start your conversation with the fact that many antibiotics actually started as products identified in nature, and so are not as far from natural compounds as may be frequently thought.
Some of you who have been reading this blog for a while will know how proud and passionate I am about The Nosocomial Project, which aims to use a science, technology, engineering, arts and mathematics (STEAM) approach to talk about infection and infection risks.
As part of this work, we organised a two part festival linked to AMR entitled Rise of the Resistance Festival. All of the content is split across YouTube and the website. I’ve included linked here in case any of it is useful in your own settings when you are looking for inspiration or planning content. The content covered in the festival included everything from a play aimed at pre-school aged children entitled Sock the Puppet, who is a hand puppet who is scared of germs, expert panels, comedy sets, and Klebsiella as a drag queen. I still have so much fun rediscovering this content, and I hope you’ll feel the same way.
I would make a plea that we all work together on this one to do some myth busting and get messages about AMR out there, but also find a way to get messages across that are entertaining/joyous and filled with hope for what we can achieve, rather than focusing on the horrors of what happens if we don’t get our act sorted. I think all of us, including healthcare professionals, have had our fill of trauma in the last few years. So, let’s focus on empowerment and positivity to make this change happen, rather than following in the footsteps of those who want a world of decisions driven by fear.
All opinions in this blog are my own


[…] Awareness Week 2023: Thinking differently about ‘Super Wicked’ problems Let’s Talk Antimicrobial Resistance for World Antimicrobial Awareness Week (WAAW) 2024 […]
LikeLike
[…] used so that I am able to see if a bacteria will respond to an antibiotic, by seeing if they carry antibiotic resistance genes, which can be crucial to getting patients on the right treatment at the right […]
LikeLike